
There is a huge dearth of cleanliness in India--open defecation is rampant; garbage management in most cities is in shambles; toxic hospital and industrial wastes and sewage are allowed to drain into water sources and food products are laced with chemicals.
However, we still seem to be oblivious to the much more dangerous consequence of this incessant poisoning of our water, soil and environment and its impact on health and survival. For lurking behind the filth are superbugs or antibiotic resistant bacteria.
Superbugs, killers in disguise!
Life was difficult at a time when simple bacterial infections could kill a person if he or she was not immune enough. Antibiotics were miracle drugs that were found to be effective against infections by killing bacteria and restoring health.
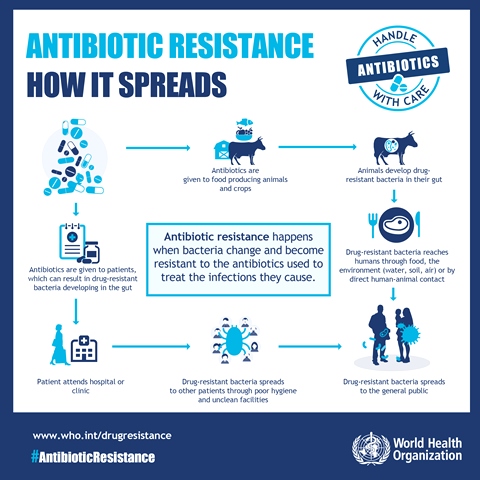
Dr Sampada Patwardhan, clinical microbiologist from Deenanath Mangeshkar hospital says, “Microorganisms such as bacteria have a remarkable capacity to adapt and survive in adverse environments. Antibiotic resistance arises when such bacteria evolve mechanisms to withstand or resist the effects of antibiotics targeted to destroy them and fight infection by changing themselves. They can do so by secreting enzymes that can inactivate the antibiotic, change the permeability of their cell membranes to prevent entry of the antibiotic etc. These microorganisms that develop resistance to multiple antibiotics are also referred to as ‘superbugs’.”
When superbugs develop resistance to a particular antibiotic used to treat infections like say diarrhoea, the antibiotics can become ineffective. This will result in the person continuing to suffer from the condition which could even become fatal, increasing the risk of spread to others.
Should India be worried?
The situation is indeed alarming! It is estimated that 58,000 neonatal deaths are caused due to drug resistance to first-line antibiotics each year in India and the problem is growing.
“Carbapenems and Colistin are the last-resort antibiotics that are used to treat serious bacterial infections in humans. However, a number of bacteria such as E. coli, Klebsiella pneumoniae, Acinetobacter baumannii and Pseudomonas aeruginosa that cause infections like diarrhoea, pneumonia, meningitis etc are showing growing resistance to these antibiotics. This can have extremely serious consequences and render some of the infections incurable,” says Dr Patwardhan.
Water and food harbour superbugs
Believe it or not, water and food are two important sources of superbugs in India, besides factors such as over-prescription and overuse or erratic use of antibiotics in health care settings! How does this happen?

Water sources in India are highly contaminated
Sixty two million tonnes of waste is generated each year in India. One of the worst Indian nightmares is the lack of systematic mechanisms to segregate and process this waste which is a dangerous concoction of dry plastic, papers, cartons, metals, along with rotting food items, as well as bandages, linen, soiled sanitary products and other infectious waste.
Many-a-times, this waste is collected in a mixed form, transported and disposed off without being adequately processed and often gets released into the water and soil, polluting it.
Open defecation is common and a large proportion of people in the country still relieve themselves in the open--in the fields, behind trees, on the roadside, railway tracks and river banks leading to faecal contamination of water and soil. Effluents from pharmaceutical industries and hospitals and sewage generated in the cities are often released untreated into the water sources. Industrial and hospital effluents often contain large amounts of antibiotic residues.
Polluted water breeds superbugs
The untreated sewage and effluents that are released into the water and soil are laden with various disease producing bacteria that develop antibiotic resistance due to prolonged exposure to antibiotics present in the industrial and hospital effluents.
Not only rivers, streams, ponds and lakes, but even groundwater has been found to harbour antibiotic resistant bacteria at different sites in India. Recent studies show that rivers such as the Ganga, Yamuna, Cauvery and Mutha are highly polluted and harbour bacteria with high levels of resistance to broad spectrum antibiotics. Water samples taken from rivers and sewage treatment plants (STPs) from Bihar, Goa, Karnataka, Tamil Nadu, and Telangana found E. coli in the waters that were resistant to antibiotics.
Drinking water collected from rivers, kunds, ponds, tube wells, hand pumps, piped supply, and dug wells in Ayodhya-Faizabad, located on the banks of the river Saryu and water sources from east Sikkim showed that bacteria such as E. coli and Klebsiella species were resistant to the latest antibiotics. Analysis of water sources from streams, lakes, tube wells, and community supplied water in Kashmir also showed that E. coli was resistant to antibiotics.
Tap water, borewell water and water from rivers and lakes, water sources contaminated by sewage treatment plants, and surface water near drug manufacturing units in Hyderabad were found to have antibiotic resistant bacteria in the waters. Wastewater samples from sewage treatment plants (STPs) in South India showed that hospital wastewater inflow led to increase in drug resistant bacteria.
Animal food too harbours superbugs
Samples from food products such as poultry, fish, eggs, milk have also been found to harbour antibiotic resistant bacteria. This is because low doses of antibiotics are routinely used as growth promoters in livestock in India.
Antibiotic resistant bacteria were found in fresh herbs and vegetables imported from India to Switzerland and raw chicken, meat, egg and unpasteurised milk samples from Hyderabad. Studies from poultry, shrimp farms of Andhra Pradesh, Karnataka, Kerala, and Tamil Nadu, milk samples from livestock in Tamil Nadu, fish samples from Kerala, Karnataka and West Bengal also found antibiotic resistant bacteria in the food samples tested.
Superbugs can spread rapidly
Bacterial resistance can spread rapidly as superbugs can multiply fast and make other bacteria found in food and water, resistant to antibiotics. Superbugs can be transferred to humans through a number of modes such as direct contact with animal handlers, live animals and animal carcasses at poultry farms and slaughterhouses; consumption of meat, chicken, fish, eggs and milk contaminated with antibiotic resistant bacteria; and environmental contamination of soil, water and air through human excreta, animal droppings and farm waste.
Poor sanitation and hygiene and WASH practices among individuals who are carriers of superbugs can also facilitate spread of superbugs in the community, household and healthcare settings.
How well is India prepared to deal with the crisis?
On April 2017, a five-year National Action Plan was released by the health ministry to tackle the problem of antibiotic resistance in the country. Experts argue that the implementation task force for this plan needs maximum support and resources from the government as the current standing and preparation of India against this challenge is dangerously inadequate.
No legislative provisions exist to prevent use of antibiotics in livestock and poultry and dairy products in India and no standards have been framed by the Central Pollution and Control Board (CPCB) yet for pharmaceutical industries to prevent antibiotic residues in industrial effluents from entering the water bodies and the environment.
Dr S. Ghosh, a senior scientist from Pune working on alternate therapies to antibiotic usage says, “Drug manufacturers, livestock and poultry producers, hospitals and healthcare facilities are some of the superbug hotspots and major polluters of the environment. Strong legislation and a highly effective regulatory system need to be put in place urgently to prevent the spread of superbugs by involving stakeholders at different scientific, social, legal and policy levels.”
He believes that conducting systematic clinical and epidemiological studies within these hotspots through routine surveillance of drug resistant bacteria in water, food, humans, animals and the environment is also important to find an appropriate solution to the problem. “For this, we need to develop strict screening and monitoring protocols for different situations and contexts within these hotspots,” he says.
“At the same time, increasing awareness among the public on the threat of drug resistant bacteria, overuse of antibiotics, the role of good sanitation and hygiene and WASH practices, needs to be our first priority to prevent spread of superbugs in the country,” he adds.
No longer can we turn our backs to the basic principle that good health is often based on access to clean food, water and environment and not medicines.
Microbiologist Dr Camilla Rodrigues, chairperson of P.D. Hinduja Hospital’s infection control committee says that there is more emphasis on prescribing antibiotics and less on infection control at present in India. More emphasis on infection control by focusing on sanitation and bringing down use of antibiotics will reduce antibiotic resistance. “The sanitation connection, though overlooked, is elementary: cleaner surroundings both in the community as well in hospitals can check the incidence of infectious diseases and bring down drug use,” she says.
It is time we shift our attention from quick fix solutions to addressing the root cause of the superbug problem--better sanitation and a clean environment.