
While the monsoons are eagerly awaited in the country, India's health system remains stretched while struggling with the Covid-19 pandemic. This is a time when vector borne diseases could become rampant, and neglect of preventive measures could lead to a spike in these diseases, warn experts!
Water and vector borne diseases are inexplicably linked as stagnant polluted water, water collected in pots and pans, old tyres, constructions sites, puddles, water logging due to rainfall aids breeding of mosquitoes and the eggs, larvae and pupae of the mosquitoes need water for their survival. Adult mosquitoes - one of the important culprits that spread some of the deadliest vector borne diseases in India, emerge out of the water and live on human blood. Read further to know more on how this happens and what needs to be done to deal with it.
What are vector borne diseases?
Vector borne diseases are a group of diseases that are caused by parasites, viruses and bacteria transmitted through vectors - living organisms that can transmit these infectious pathogens (parasites, virus, bacteria) from one human to another, or from animals to humans.
Vectors mainly include insects like mosquitoes, ticks, fleas, lice that depend on the blood of humans and animals, and can ingest disease producing microorganisms while sucking blood from an infected host (human or animal) and later transmit it into a new host, after the disease producing pathogen has replicated. Once a vector becomes infectious, it can keep on transmitting the pathogen for the rest of its life during each subsequent bite/blood meal.
What are the types of vector borne diseases?
Table Source: World Health Organisation (2020) Vector Borne diseases. Factsheets
The common vector borne diseases include:
Dengue:
Dengue is a mosquito-borne viral disease that spreads through the bite of an infected Aedes mosquito. The virus responsible for causing dengue, is called dengue virus (DENV). There are four strains of DENV virus, which increase the possibility of people being infected four times due to different strains of the virus. While many DENV infections produce only mild illness, some can cause an acute flu-like illness that can develop into a lethal complication, called severe dengue, which is a leading cause of serious illness and deaths in some Asian and Latin American countries.
The most common symptoms of dengue include fever with headaches, nausea, vomiting, rash, eye pain, muscle and joint pain, bone pain, swollen glands. Dengue stays for about 2 to 7 days. There is no specific medication to treat dengue.
The best preventive measure for dengue is to avoid mosquito bites through use of personal protective measures such as nets, mosquito repellent creams and most importantly taking measures to prevent mosquito breeding sites by avoiding indoor and outdoor collection of water in pans, pots, bottles, tyres etc that can breed mosquito eggs and larvae.
Read more about dengue here
Malaria:
Malaria is caused by Plasmodium parasites. The parasites are spread to people through the bite of infected female Anopheles mosquito. There are 5 parasite species that cause malaria in humans, and two of these species, namely P. falciparum and P. vivax pose the greatest threat. Symptoms usually appear 10–15 days after the infective mosquito bite and include fever, headache, and chills. If not treated within 24 hours, malaria caused by the bite of P. falciparum can progress to severe illness, often leading to death.
Malaria prevention involves attempts to control the vector mainly through use of personal protective equipment such as mosquito nets and use of chemical sprays besides measures to prevent accumulation of stagnant water in potholes, ditches, ponds etc that can breed mosquito larvae.
Read more here
Chikungunya
Is a mosquito borne viral disease transmitted through the bite of an infected female mosquitoe namely Aedes aegypti and Aedes albopictus. Symptoms appear within 4 to 7 days and include fever, severe joint pain that can last over days and months, headache, nausea, fatigue and rash.
There is no specific treatment for chikungunya and prevention and control include means such as reducing the number of water filled places that can breed mosquitoes.
Read more here
Japanese encephalitis (JE)
Is a mosquito borne viral disease. Most Japanese Encephalitis virus (JEV) infections are mild (fever and headache) or without apparent symptoms. In children, gastrointestinal pain and vomiting can be the initial symptoms while severe disease is characterised by rapid onset of high fever, headache, neck stiffness, disorientation, coma, seizures, spastic paralysis and ultimately death. As high as 30 percent deaths can occur among those with disease symptoms. Of those who survive, 20–30 percent can suffer permanent intellectual, behavioural or neurological damage such as paralysis, recurrent seizures or the inability to speak.
The World Health Organisation (WHO) recommends strong JE prevention and control activities, including immunisation in all regions where the disease is a public health priority, along with strengthening surveillance and reporting mechanisms. Major outbreaks of JE occur every 2-15 years. JE transmission intensifies during the rainy season, during which vector populations increase. The spread of JEV has also been correlated to agricultural development and intensive rice cultivation supported by irrigation programmes, in recent years.
Read more here
Lymphatic Filariasis
Is caused by infection with parasites classified as nematodes (roundworms) that are transmitted through the bite of infected mosquitoes. Adult filarial worms can cause inflammation and dysfunction of the lymphatic system, which leads to recurrent bacterial infections in the lower limbs. These infections can lead to local pain and swelling accompanied with fever and chills. The swelling on the lower limbs in its advanced form is referred to as elephantiasis which is severely disabilitating and can restrict people from carrying out their daily activities. Prevention of mosquito bites, treatment of symptoms and management of disability are the ways to deal with the disease.
Read more here
Kala Azar or Leishmaniasis
Is caused by Leishmania parasites which are transmitted through the bite of infected female phlebotomine sandflies. The disease mainly affects the poor and is associated with malnutrition, population displacement, poor housing, a weak immune system and lack of financial resources.
There are three types of leishmaniasis – visceral (also known as kala-azar, which is and the most serious form of the disease), cutaneous (the most common), and mucocutaneous. Visceral leishmaniasis (VL), also known as kala-azar is fatal if left untreated in over 95 percent of cases. It involves irregular bouts of fever, weight loss, enlargement of the spleen and liver, and anaemia. It is commonly found in Brazil, East Africa and in India. Early diagnosis and treatment and decreasing the number of sandflies through use of insecticidal sprays, nets can help in reducing the risk of the disease.
Read more here
Know more about other vector borne diseases here
What is the distribution of vector borne diseases globally?
Vector-borne diseases account for more than 17 percent of all infectious diseases globally.More than 700, 000 deaths occur annually due to vector-borne diseases such as malaria, dengue, schistosomiasis, human African trypanosomiasis, leishmaniasis, chagas disease, yellow fever, japanese encephalitis and onchocerciasis.
Vector borne diseases disproportionately affect poorer populations that live in degraded environments and poor housing conditions. Malaria causes an estimated 219 million cases globally, and results in more than 400,000 deaths every year. Most of the deaths occur in children under the age of 5 years. Dengue is the most prevalent viral infection transmitted by Aedes mosquitoes. More than 3.9 billion people in over 129 countries are at risk of contracting dengue, with an estimated 96 million symptomatic cases and an estimated 40,000 deaths every year. Japanese encephalitis virus is the cause of viral encephalitis in many Asian countries leading to around 68,000 clinical cases every year. There has been a rise in chikungunya cases in Asia in the last few years with India, Indonesia, Maldives, Myanmar and Thailand having reported over 1.9 million chikungunya cases since 2005.
Read more here
What are the common vector borne diseases in India?
The common vector borne diseases in India include malaria, dengue, chikungunya, encephalitis, kala-azar, filariasis. According to the National Health Profile 2019 by the Central Bureau of Health Intelligence, Government of India, while malaria has been a problem in India for centuries, the prevalence of the disease has decreased in 2012 and 2013, with a slight increase in 2014 & 2015 followed by a decline from 2016. While malaria has showed a dip in India in 2017-2018, it accounted for 85 percent of deaths in the year. In 2018, maximum number of cases and deaths due to malaria were reported in Chattisgarh.
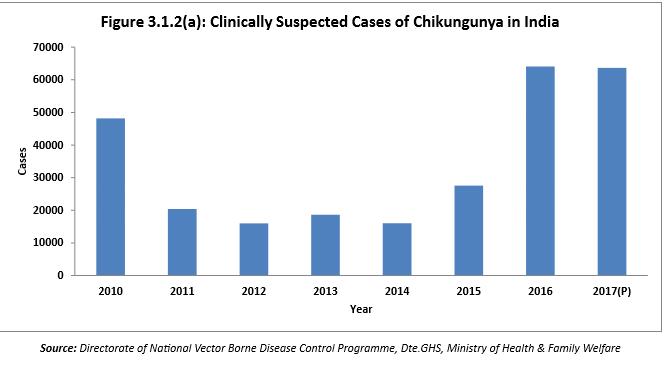
Kala-azar is the second largest killer world over and the parasite Leishmania donovani causes this disease in India with Bihar accounting for maximum number of cases. Dengue and Chikungunya transmitted by Aedes mosquitoes are a cause of great concern to public health in India. Every year, thousands of individuals are affected and contribute to the burden of health care.
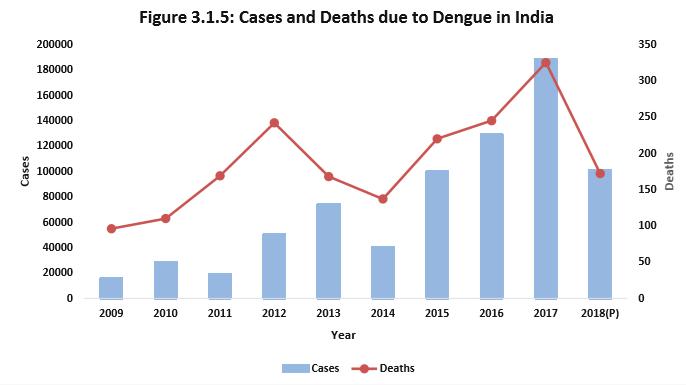
Dengue outbreaks have continued since the 1950s, but severity of disease has increased in the last two decades. Reported cases of chikungunya in the country have shown a slight decrease in 2018 as compared to 2017. However, total number of cases and deaths due to encephalitis continue to be high in the country with Assam reporting maximum numbers of cases and deaths.
Read more here
Why are vector borne diseases rampant in India? Why are they more common in the monsoons?
The relationship between the rains and rise in vector borne diseases due to increase in number of vectors is complex and context specific. For example, increased rainfall can provide more vector breeding sites, but drought too can provide more breeding sites due to an increase in the use of containers for rainwater collection and storage, which are breeding sites for A. aegypti. Increase in number of vectors is also influenced by changes in the ecosystem coupled with climate change, which could degrade or enhance vector habitats, encourage competition betwenn species for survival making the virus more aggressive, or it could increase or reduce the number of vector predators or vector pathogens.
Although unseasonal rains have been found to trigger the epidemic, rapid and unplanned development and urbanisation leading to poor housing conditions, increase in construction site activities, irregular water supply and water storage practices, poor environmental sanitation, inefficient garbage management practices, use of plastic bags and containers by people etc. are adding to the spread of diseases such as dengue in India. Lack of awareness also worsens the situation and behavioural factors such as leaving small pots and pans filled with water in or near houses, storing large quantities of water due to the irregular availability of water etc., have also been found to trigger the spread of the disease as mosquitoes can breed in stored uncovered water. In cities, people from high rise buildings and posh apartments have also been found to prevent health workers from visiting their flats for preventive fogging, triggering an increase in mosquitoes.
How will climate change impact incidence and prevalence of vector borne diseases?
Climate change has led to increase in the average surface temperature of the globe by up to 0.65 °C during last 50 years and acelerated the rate of warming along with increase in extreme rainfall events in many parts of the globe and in India, which is expected to be highly affected by the impacts of climate change.
Higher temperatures are known to increase the transmission of vector borne pathogens mainly through increasing vector numbers, pathogen replication and vector biting rate, and reducing the incubation period or the time between a vector feeding on an infected host and being able to transmit the pathogen.
Mosquito species such as the Anopheles gambiae complex, A. funestus, A. darlingi, Culex quinquefasciatus and Aedes aegypti are responsible for transmission of most vector-borne diseases and are very sensitive to temperature changes in the larval as well as adult stage. Thus if water temperature rises, the larvae take a shorter time to mature and develop a greater capacity to reproduce during the transmission period. In warmer climates, adult female mosquitoes digest blood faster and feed more frequently, thus increasing transmission intensity. Malaria parasites and viruses complete incubation within the female mosquito in a shorter time as temperature rises, thereby increasing the proportion of infective vectors.
Besides climate change, a number of social and environmental factors such as how pathogens adapt and change, the availability of vectors, urbanisation, land use, land cover, biodiversity, changing ecosystems, industrial and agricultural pollution and increase in hormone disruptive chemicals, trade and travel, demographics, human behavior, adaptive capacity, poor socioeconomic conditions, lack of infrastructural facilities leading to poor sanitation and hygiene, overcrowding, poor enviroment also interact with climate change leading to increase in the incidence of vector borne diseases.
Read more here
How can they be prevented?
While treatment for vector borne diseases is mainly provided to relieve symptoms in extreme cases, prevention is one of the most important means to prevent spread of the diseases. Vector borne diseases can be prevented by:
Reducing the source where mosquitoes breed by:
- Preventing stagnant water from accumulating around the house and in the surroundings
- Cleaning blocked drains
- Disposing tins, vesseals, containers, tyres that can accumulate water and help in mosquito breeding
- Keeping water tanks and containers tightly closed
- Filling ditches to prevent mosquito breeding
Killing mosquito and larva
- Biological control by introducing small fish such as guppies that feed on mosquito larvae
- Pouring oil over water surfaces
- Spraying of DDT, malathion, pyrethrum inside the house, especially on the walls and corners where mosquitoes are commonly found
- Wearing clothes that cover the body
- Using mosquito nets
- Using mosquito repellents
What are the health policies and programmes directed at vector borne disease control in India?
The National Vector Borne Disease Control Programme (NVBDCP) is a comprehensive programme that deals with prevention and control of vector borne diseases in India namely malaria, filaria, kala-azar, dengue and Japanese Encephalitis (JE). The Directorate of NVBDCP is the nodal agency for the implementation of the programme with respect to prevention and control and provides technical assistance and financial support to various states/UTs.
Launched in 2003-04, the NVBDCP has been formed by merging National anti -malaria control programme, National Filaria Control Programme and Kala Azar Control programmes, and Japanese Encephalitis and Dengue/DHF have also been added to the list. The Program Directorate of National Anti Malaria Programme (NAMP) is the nodal agency for prevention and control of major Vector Borne Diseases.
Vector Borne Diseases Control Programme Legislations include:
- National Anti - Malaria programme
- Kala - Azar Control Programme
- National Filaria Control Programme
- Japanese Encephilitis Control Programme
- Dengue and Dengue Hemorrhagic fever
While India’s central government is responsible for all policy making and fund allocation, the individual state governments are responsible for implementation of policies put in place by the central government and the proper utilisation of funds. However, a number of gaps in implementation at the policy level exist that include:
- Use of ineffective vector borne disease control measures
- Failure of central and state governments in providing adequate allocation and utilisation of funds
- Lack of availability of qualified staff and utilisation of informed research
- Underreporting of cases and ineffective surveillance mechanisms
- Lack of schemes to counter vector borne diseases in rural areas
- Lack of co-ordination between ministries and state agencies is a major probelm with implementation of the programme, which ideally needs to coordinate with other government agencies. For example, The Union Ministry of Drinking Water and Sanitation needs to ensure of clean surroundings and access to good quality water for consumption, The Union Ministry of Human Resource Development can build awareness among students. Research agencies involved need to find causes of the diseases and solutions. However, most ministries work in isolation, thus missing a holistic approach to reduce vector borne diseases.
What needs to be done to change this situation:
- Establishing Standard Operating Procedures (SOPs) to prevent vector borne diseases
- Fixing accountabilities between central and state governments
- Assimilation of relevant lessons from other countries
- Understanding the role of climate change in countering vector borne diseases
While monsoons continue to play truant in many parts of the country, being well prepared and to act fast and with conviction is the need of the hour in these challenging times when Covid-19 continues to cast its shadow in dealing with other types of health problems in the country.